Diabetic pancreas cells made to produce insulin by bone protein
especiales
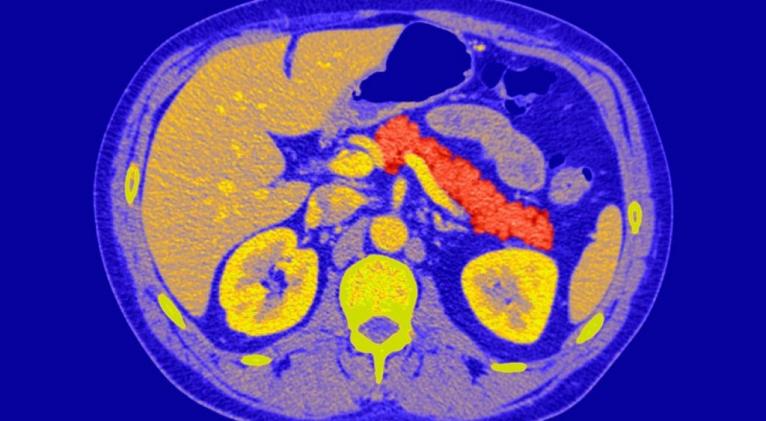
In type 1 diabetes, beta cells in the pancreas that make insulin – the hormone that keeps our blood glucose levels at a safe concentration – are destroyed by the immune system. As a result, people with the disease have to inject themselves daily with insulin.
Now, researchers have discovered that non-beta cells in the pancreas can be transformed into insulin-producing cells, merely by exposing them to a growth factor called BMP-7.
“We are very encouraged by the simplicity of our finding,” says Juan Domínguez-Bendala, director of stem cell development at the Diabetes Research Institute in Miami, Florida.
Surprise discovery
Domínguez-Bendala, who led the team along with colleague Ricardo Pastori, found that BMP-7 caused pancreatic cells to secrete unexpectedly high amounts of insulin after they used it as a control in another, unrelated, experiment.
Intrigued, they added the growth factor to a soup of pancreatic cells that do not normally produce insulin. Clumps of cells formed, which produced high amounts of insulin, and secreted even more when exposed to glucose – just as you would expect from beta cells in healthy individuals.
When the team transplanted the cells into diabetic mice whose own beta cells had been destroyed artificially with a chemical, the cells acted like healthy beta cells.
Ultimately, the team hopes to inject BMP-7 directly into the pancreas to stimulate the creation of new beta cells, allied with a small amount of immunosuppressive drugs to stop the new insulin factories being destroyed by the immune system. “If we can stimulate them in the body, that’s where the major potential is,” says Domínguez-Bendala. “We’re trying that right now in mice.”
Bigger donations
Another possibility would be to create new beta cells from donated pancreases, and package them into materials that shield the cells from the immune system. You can then implant these in a jelly-like structure in the abdomen called the omentum.
Beta cells donated from deceased individuals have already been transplanted into diabetic patients through a procedure called the Edmonton protocol. However, since beta cells make up only two per cent of a donor’s pancreas, they only provide enough cells to transplant into one person, meaning that demand far outweighs supply. And while some recipients have been able to avoid insulin injections for a decade or more, the effect of the cells has worn off after two and a half years in others.
At the very least, Domínguez-Bendala hopes that they could use BMP-7 to convert the other 98 per cent of donor pancreas cells into beta cells, which, he estimates, could potentially provide enough insulin-producing cells to transplant into seven people.
Less risk
The team believes that whichever way BMP-7 is used, it will be less risky than other treatments for type 1 diabetes that are currently being investigated, such as those that create pancreatic cells from stem cells, or by introducing new genes into the body.
Alasdair Rankin, director of research at charity Diabetes UK, says that improving the number and viability of cells for transplantation is a major focus of research here and around the world. “This study describes a promising approach in an exciting field, but it will be some years before we know whether it will be effective in medical practice,” he says.
Journal reference: Diabetes, in press











Add new comment