Blood test shows promise for early detection of severe lung-transplant rejection
especiales
Researchers have developed a simple blood test that can detect when a newly transplanted lung is being rejected by a patient, even when no outward signs of the rejection are evident. The test could make it possible for doctors to intervene faster to prevent or slow down so-called chronic rejection -- which is severe, irreversible, and often deadly -- in those first critical months after lung transplantation. Researchers believe this same test might also be useful for monitoring rejection in other types of organ transplants. The work was funded by the National Heart, Lung, and Blood Institute (NHLBI), part of the National Institutes of Health.
The study's findings are scheduled to appear Jan. 22 in EBioMedicine, a publication of The Lancet.
"This test solves a long-standing problem in lung transplants: detection of hidden signs of rejection," said Hannah Valantine, M.D., co-leader of the study and lead investigator of the Laboratory of Organ Transplant Genomics in the Cardiovascular Branch at NHLBI. "We're very excited about its potential to save lives, especially in the wake of a critical shortage of donor organs."
The test relies on DNA sequencing, Valantine explained, and as such, represents a great example of personalized medicine, as it will allow doctors to tailor transplant treatments to those individuals who are at highest risk for rejection.
Lung transplant recipients have the shortest survival rates among patients who get solid organ transplantation of any kind -- only about half live past five years. Lung transplant recipients face a high incidence of chronic rejection, which occurs when the body's immune system attacks the transplanted organ. Existing tools for detecting signs of rejection, such as biopsy, either require the removal of small amounts of lung tissue or are not sensitive enough to discern the severity of the rejection. The new test appears to overcome those challenges.
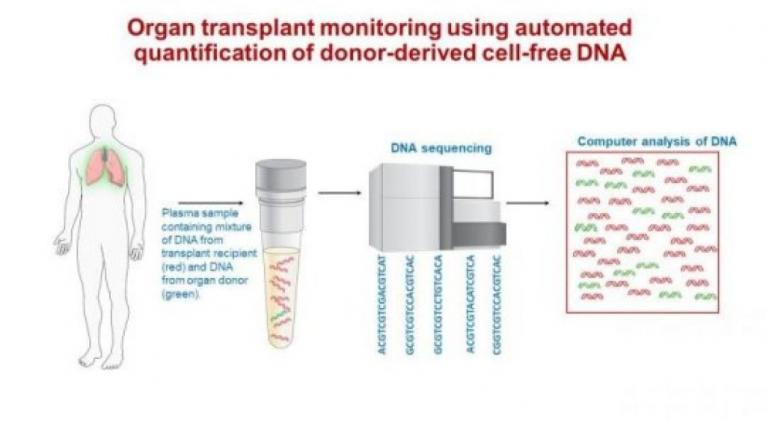
Called the donor-derived cell-free DNA test, the experimental test begins with obtaining a few blood droplets taken from the arm of the transplant recipient. A special set of machines then sorts the DNA fragments in the blood sample, and in combination with computer analysis, determines whether the fragments are from the recipient or the donor and how many of each type are present. Because injured or dying cells from the donor release lots of donor DNA fragments into the bloodstream compared to normal donor cells, higher amounts of donor DNA indicate a higher risk for transplant rejection in the recipient.
In the study, 106 lung transplant recipients were enrolled and monitored. Blood samples collected in the first three months after transplantation underwent the testing procedure. The results showed that those with higher levels of the donor-derived DNA fragments in the first three months of transplantation were six times more likely to subsequently develop transplant organ failure or die during the study follow-up period than those with lower donor-derived DNA levels. Importantly, researchers found that more than half of the high-risk subjects showed no outward signs of clinical complications during this period.
"We showed for the first time that donor-derived DNA is a predictive marker for chronic lung rejection and death, and could provide critical time-points to intervene, perhaps preventing these outcomes," Valantine said. "Once rejection is detected early via this test, doctors would then have the option to increase the dosages of anti-rejection drugs, add new agents that reduce tissue inflammation, or take other measures to prevent or slow the progression."
In 2010, Valantine was part of a research team that pioneered the first blood test to diagnose organ rejection. The now-widely used test, called the AlloMap, analyzes the expression of 20 genes in a transplant recipient's blood sample to determine whether the patient's immune system is launching an attack. The following year, Valantine and her colleagues showed for the first time that a cell-free DNA blood test could be useful for monitoring early signs of rejection. However, those early studies of the cell-free DNA test only identified signs of "acute" transplant rejection, which is easily reversed. The current study shows that high cell-free DNA levels during the first three months after transplant predicts chronic rejection. If validated, this blood test could become a routine tool used to monitor transplant patients at very early stages of rejection, the researchers said.
This research is supported by The Genomic Research Alliance for Transplantation Study (NCT02423070), which is funded by the Division of Intramural Research of NHLBI. The research is also supported by The Genome Transplant Dynamics Study (NCT01985412), which is funded by the National Institute of Allergy and Infectious Diseases through Grant RC4AI092673.











Add new comment